Trigeminal Neuralgia-
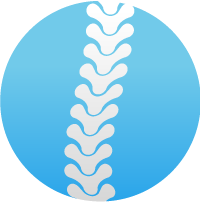
Trigeminal neuralgia (TN), also called tic douloureux, is a chronic pain condition that causes extreme, sporadic, sudden burning or shock-like face pain. The pain seldom lasts more than a few seconds or a minute or two per episode. The intensity of pain can be physically and mentally incapacitating. TN pain is typically felt on one side of the jaw or cheek. Episodes can last for days, weeks, or months at a time and then disappear for months or years. In the days before an episode begins, some patients may experience a tingling or numbing sensation or a somewhat constant and aching pain. The attacks often worsen over time, with fewer and shorter pain-free periods before they recur.
The intense flashes of pain can be triggered by vibration or contact with the cheek (such as when shaving, washing the face, or applying makeup), brushing teeth, eating, drinking, talking, or being exposed to the wind. TN occurs most often in people over age 50, but it can occur at any age, and is more common in women than in men. There is some evidence that the disorder runs in families, perhaps because of an inherited pattern of blood vessel formation. Although sometimes debilitating, the disorder is not life-threatening.
The presumed cause of TN is a blood vessel pressing on the trigeminal nerve in the head as it exits the brainstem. TN may be part of the normal aging process but in some cases it is the associated with another disorder, such as multiple sclerosis or other disorders characterized by damage to the myelin sheath that covers certain nerves.
Treatment-
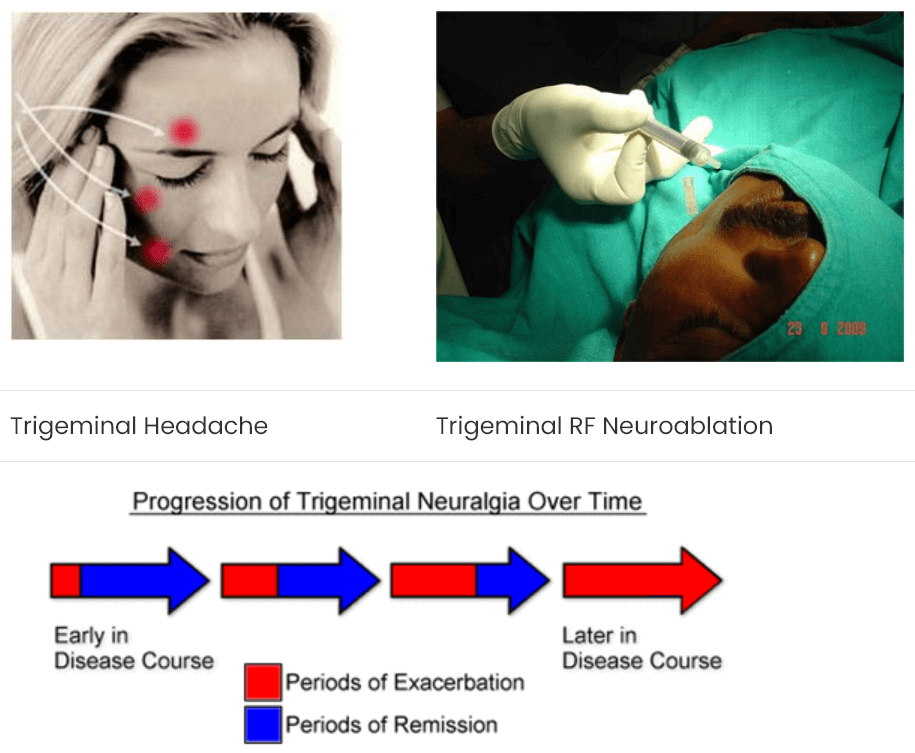
Because there are a large number of conditions that can cause facial pain, TN can be difficult to diagnose. But finding the cause of the pain is important as the treatments for different types of pain may differ. Treatment options include medicines such as anticonvulsants and tricyclic antidepressants, surgery, and complementary approaches. Typical analgesics and opioids are not usually helpful in treating the sharp, recurring pain caused by TN. If medication fails to relieve pain or produces intolerable side effects such as excess fatigue, Interventional Pain Treatment is recommended done on an outpatient basis in which TN is blocked by Neurolytic drug or Radiofrequency with good results. As a last resort several neurosurgical procedures are available which are more complex and require hospitalization. Some patients choose to manage TN using complementary techniques, usually in combination with drug treatment. These techniques include acupuncture, biofeedback, vitamin therapy, nutritional therapy, and electrical stimulation of the nerves.
Prognosis-
The disorder is characterized by recurrences and remissions, and successive recurrences may incapacitate the patient. Due to the intensity of the pain, even the fear of an impending attack may prevent activity. Trigeminal neuralgia is not fatal.
Post Herpetic Neuralgia-
PHN is a neuralgia, nerve damage caused by the varicella zoster virus. Typically, the neuralgia is confined to a dermatome area of the skin and follows an outbreak of herpes zoster (HZ, commonly known as shingles) in that same dermatome area. The neuralgia typically begins when the HZ vesicles have crusted over and begun to heal, but it can begin in the absence of HZ rash. The damage causes nerves in the affected dermatomic area of the skin to send abnormal electrical signals to the brain. These signals may convey excruciating pain, and may persist or recur for months, years or until death.
Treatment options for PHN include antidepressants, anticonvulsants (such as gabapentin or pregabalin) and topical agents such as lidocaine patches or capsaicin lotion. Opioid analgesics may also be appropriate in many situations. There is role of PRF (Pulsed Radiofrequency) and TENS (a type of electrical pulse therapy).


Diabetic Neuropathy
Diabetic neuropathies are neuropathic disorders that are associated with diabetes mellitus. These conditions are thought to result from diabetic microvascular injuryblood vessels that supply nerves (vasa nervorum) in addition to macrovascular conditions that can culminate in diabetic neuropathy. Relatively common conditions which may be associated with diabetic neuropathy include third nerve palsy; mononeuropathy; mononeuropathy multiplex; diabetic amyotrophy; a painfulautonomic neuropathy; and thoracoabdominal neuropathy. involving small polyneuropathy;
Diabetic neuropathy affects all peripheral nerves: pain fibers, motor neurons, autonomic nerves. It therefore necessarily can affect all organs and systems since all are innervated. There are several distinct syndromes based on the organ systems and members affected, but these are by no means exclusive. A patient can have sensorimotor and autonomic neuropathy or any other combination. Symptoms vary depending on the nerve(s) affected and may include symptoms other than those listed. Symptoms usually develop gradually over years.